Trauma profoundly impacts brain structure and function, altering memory, emotion regulation, and cognitive processes; Understanding this connection is key to effective recovery and support strategies.
What is Trauma?
Trauma refers to a person’s emotional, psychological, or physiological response to a distressing event, such as abuse, accidents, or violence. It disrupts normal brain functioning, particularly in regions like the amygdala, hippocampus, and prefrontal cortex. Traumatic experiences can be acute or chronic, leaving lasting imprints on memory, emotional regulation, and behavior. The brain’s alarm system, the amygdala, becomes hyperactive, while the prefrontal cortex may underperform, affecting decision-making and emotional control. Trauma can also alter brain development in children, leading to long-term mental and physical health challenges. Understanding trauma is crucial for addressing its impact and fostering recovery through targeted therapies and support strategies.
The Impact of Trauma on Brain Function
Trauma disrupts normal brain processes, particularly in regions like the amygdala, hippocampus, and prefrontal cortex. The amygdala becomes hyperactive, triggering intense fear responses, while the hippocampus struggles to process and store traumatic memories, leading to fragmented recollections. The prefrontal cortex, responsible for executive functioning, may underperform, impairing decision-making and emotional regulation. This imbalance can result in heightened stress responses, flashbacks, and emotional dysregulation. Over time, chronic trauma may rewire brain circuits, affecting mental health and behavior. Understanding these changes is essential for developing effective interventions to restore brain function and promote recovery.
The Importance of Understanding Trauma and the Brain
Understanding trauma’s impact on the brain is crucial for effective support and recovery. It helps professionals and caregivers develop trauma-informed strategies, fostering safer environments for healing. By recognizing how trauma alters brain function, interventions can target specific areas, improving emotional regulation and cognitive processes. This knowledge also reduces stigma, promoting empathy and compassion. Ultimately, understanding trauma’s neurological effects is key to helping individuals regain control over their lives and achieve long-term well-being.

The Neurobiology of Trauma
Trauma triggers biological changes in the brain, affecting regions like the amygdala, hippocampus, and prefrontal cortex. It disrupts normal functioning, altering emotional responses and memory processing.
The Role of the Amygdala in Trauma Response
The amygdala acts as the brain’s alarm system, detecting threats and triggering the fight-or-flight response. During trauma, it becomes hyperactive, intensifying emotional reactions. This heightened activation disrupts the prefrontal cortex’s ability to regulate emotions, leading to impulsive behaviors. The amygdala’s overactivity also impairs the hippocampus’s memory processing, resulting in fragmented or distorted trauma memories. Over time, this can contribute to conditions like PTSD, where the amygdala remains overly sensitive, causing flashbacks or intense fear responses. Understanding the amygdala’s role is crucial for therapies like EMDR, which aim to reduce its hyperactivity and promote emotional regulation, aiding in trauma recovery and restoring balance to brain function.
The Hippocampus and Memory Processing in Trauma
The hippocampus plays a critical role in processing and storing memories, particularly emotional ones. During trauma, its function is disrupted, leading to fragmented or unprocessed memories. Normally, the hippocampus organizes memories into coherent narratives, but trauma can prevent this, causing memories to remain disjointed and distressing. This disruption is linked to conditions like PTSD, where flashbacks and nightmares recur. The hippocampus also processes memories during sleep, but trauma can impair this, leaving memories “stuck” in the brain. Understanding this helps in therapies like EMDR, which aim to reintegrate these memories, reducing their distressing impact and promoting healing. This process is vital for recovery and restoring normal brain function.
The Prefrontal Cortex and Executive Functioning in Traumatized Brains
Trauma often disrupts the prefrontal cortex, impairing executive functioning, which includes decision-making, planning, and self-regulation. This underactivation can lead to difficulties in managing emotions, focusing, and completing tasks. The prefrontal cortex, responsible for rational thinking, may struggle to override the amygdala’s emotional responses, resulting in heightened reactivity. Over time, this can affect problem-solving abilities and judgment. Traumatized individuals may also experience challenges with impulse control and maintaining goal-oriented behavior. Understanding this neural impact is crucial for developing targeted therapies to restore prefrontal function and improve overall cognitive and emotional well-being in those affected by trauma.
The Thalamus as a Gatekeeper of Information
The thalamus acts as the brain’s gatekeeper, filtering and processing sensory information before it reaches higher cortical areas. In trauma, this function can be disrupted, leading to sensory overload or fragmented processing. The thalamus plays a key role in regulating consciousness and alertness, but traumatic experiences can impair its ability to modulate information flow. This disruption may result in heightened startle responses or difficulty screening out irrelevant stimuli. Additionally, the thalamus’s role in memory formation can be affected, contributing to the development of flashbacks or nightmares. Understanding the thalamus’s role in trauma is essential for addressing sensory and cognitive challenges in recovery.

Key Brain Regions Affected by Trauma
Trauma impacts the amygdala, hippocampus, prefrontal cortex, and thalamus, disrupting emotional regulation, memory processing, and sensory integration, leading to long-term cognitive and emotional challenges.
The Amygdala: The Brain’s Alarm System
The amygdala acts as the brain’s alarm system, detecting threats and triggering the fight-or-flight response. During trauma, it activates, releasing stress hormones like adrenaline and cortisol. This process prepares the body to react but can lead to hyperactivation in traumatized individuals, causing heightened sensitivity to triggers. The amygdala’s overactivity disrupts emotional regulation, making it difficult to distinguish past threats from present safety. This hyperarousal can result in flashbacks, anxiety, and hypervigilance, significantly impacting daily life and mental health. Understanding the amygdala’s role is crucial for addressing trauma’s effects and restoring balance to the brain’s response system.
The Hippocampus: The Brain’s Librarian
The hippocampus plays a vital role in processing and storing memories, especially emotional ones. Trauma disrupts its function, preventing memories from being properly filed. This leads to fragmented recollections that resurface involuntarily, causing distressing flashbacks or nightmares. The hippocampus’s impaired ability to regulate memory consolidation results in memories remaining in an unprocessed state, making them feel as if they’re happening again. This disruption can hinder recovery and affect daily functioning. Understanding the hippocampus’s role in trauma helps in developing targeted therapies to restore its function and promote healing.
The Prefrontal Cortex: Executive Functioning and Decision-Making
The prefrontal cortex, responsible for executive functioning, decision-making, and emotional regulation, is often underactivated in traumatized brains. This impairment can lead to difficulties in planning, problem-solving, and self-control. Trauma disrupts the prefrontal cortex’s ability to regulate emotions, causing heightened emotional reactivity and impulsivity. Elevated levels of stress hormones, such as cortisol, can persist for days or months after a traumatic event, further impacting cognitive functioning. This disruption can affect daily life, making it challenging to focus, complete tasks, or make rational decisions. Understanding this connection is crucial for developing strategies to restore prefrontal cortex function and improve overall mental health.
The Anterior Cingulate Cortex: Emotional Regulation
The anterior cingulate cortex (ACC) plays a critical role in emotional regulation, error detection, and empathy. Trauma can disrupt ACC functioning, leading to emotional dysregulation and heightened sensitivity to stress. This disruption often results in difficulty managing emotions, increased emotional reactivity, and challenges in maintaining emotional balance. The ACC’s impaired function can also affect interpersonal relationships, as it struggles to regulate empathy and social responses. Understanding the ACC’s role in trauma is essential for addressing emotional regulation challenges and developing targeted therapeutic interventions to restore its function and improve overall emotional well-being.

The Effects of Trauma on Brain Development
Trauma alters brain development, particularly in children, affecting regions like the hippocampus and prefrontal cortex, leading to long-term cognitive, emotional, and mental health challenges.
Childhood Trauma and Altered Brain Development
Childhood trauma significantly impacts brain development, particularly in regions like the hippocampus and prefrontal cortex. These areas, crucial for memory and emotional regulation, may develop abnormally due to chronic stress. The hippocampus, responsible for processing memories, can reduce in volume, impairing memory and increasing anxiety and depression risks. The prefrontal cortex, which manages decision-making and self-control, may also underdevelop, leading to difficulties in regulating emotions and behaviors. Early traumatic experiences can disrupt normal brain maturation, resulting in long-term mental health challenges, such as PTSD, anxiety, and depression. Understanding these effects is essential for developing interventions to support healthy brain development and resilience in traumatized children.
The Impact of Chronic Trauma on Brain Structure
Chronic trauma can lead to significant changes in brain structure, particularly in regions like the hippocampus, amygdala, and prefrontal cortex. The hippocampus, essential for memory processing, may shrink due to prolonged stress, impairing memory and increasing vulnerability to anxiety and depression. Conversely, the amygdala, which processes fear, may enlarge, heightening sensitivity to threats. The prefrontal cortex, responsible for decision-making and emotional regulation, can also atrophy, reducing its ability to manage stress and emotions effectively. These structural changes disrupt normal brain function, leading to long-term mental health challenges. Understanding these alterations is crucial for developing targeted interventions to mitigate the effects of chronic trauma on brain health.

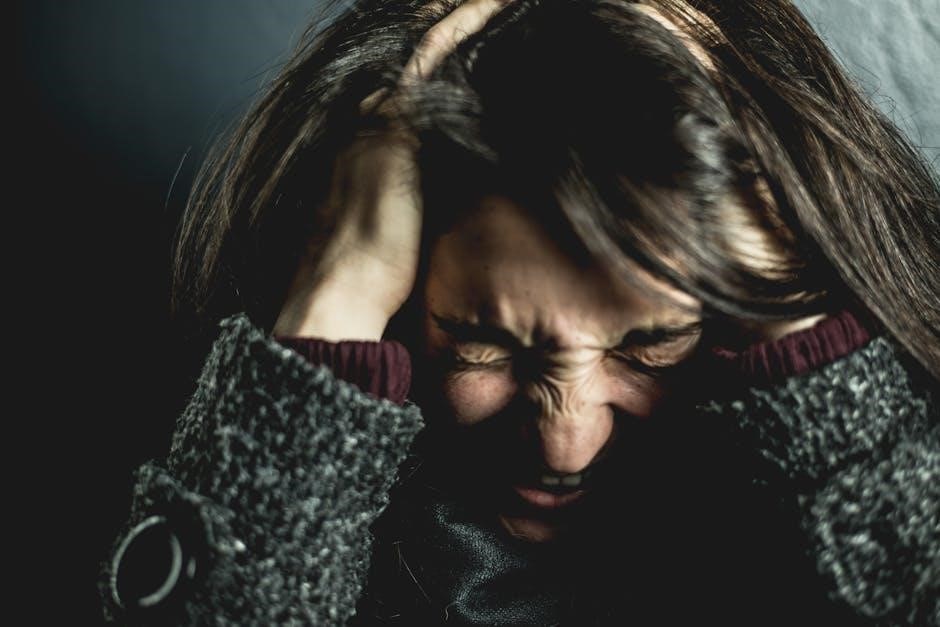
Psychological and Emotional Impact of Trauma
Trauma alters brain function, causing anxiety, depression, and emotional dysregulation. The brain’s alarm system remains active, disrupting emotional balance and mental health over time.
Post-Traumatic Stress Disorder (PTSD) and the Brain
Post-Traumatic Stress Disorder (PTSD) develops after traumatic events, deeply affecting brain regions like the amygdala, hippocampus, and prefrontal cortex. The amygdala becomes hyperactive, intensifying fear responses, while the hippocampus struggles to process memories, leading to fragmented recollections. The prefrontal cortex, responsible for emotional regulation, becomes underactive, impairing decision-making and rational thinking. This imbalance disrupts normal brain functioning, causing flashbacks, nightmares, and heightened arousal. Understanding these neurological changes is crucial for developing effective treatments, such as therapy and neuroplasticity-based interventions, to help individuals regain control over their emotions and thoughts. PTSD highlights the profound interplay between trauma, brain structure, and mental health outcomes.
Anxiety and Depression: The Role of Trauma
Trauma significantly contributes to the development of anxiety and depression by altering brain function and emotional regulation. The amygdala, hyperactivated by traumatic experiences, intensifies fear responses, while the hippocampus struggles to process memories, leading to emotional dysregulation. Elevated cortisol levels and disrupted neurotransmitter balance further exacerbate mood disorders. Trauma impairs the prefrontal cortex’s ability to regulate emotions, resulting in heightened anxiety and depressive symptoms. These changes create a cycle of distress, making it challenging to manage emotions and thoughts. Understanding the neurological impact of trauma is essential for addressing anxiety and depression effectively, emphasizing the need for targeted interventions to restore emotional balance and brain health.
Emotional Dysregulation and Trauma
Trauma often leads to emotional dysregulation by disrupting the brain’s ability to manage emotions effectively. The prefrontal cortex, responsible for regulating emotions, becomes underactivated, while the amygdala, which processes fear, becomes overactivated. This imbalance results in heightened emotional reactivity, making it difficult to calm down after distress. Trauma also impacts the anterior cingulate cortex, which helps balance emotions, leading to challenges in emotional resilience. Over time, this dysregulation can create a cycle of intense emotional responses, complicating daily life and relationships. Understanding this connection is crucial for developing strategies to restore emotional balance and promote healing in traumatized individuals.

Therapeutic Approaches to Trauma Recovery
Effective therapies like EMDR, CBT, mindfulness, and neurofeedback help rewire the brain, promoting emotional healing and restoring cognitive function in trauma survivors.
Eye Movement Desensitization and Reprocessing (EMDR) Therapy
EMDR therapy is a powerful approach to trauma recovery, helping the brain process and integrate traumatic memories. By replicating natural memory processing, EMDR reduces distress associated with traumatic events. During sessions, guided eye movements or other forms of bilateral stimulation activate the brain’s natural healing mechanisms. This process allows the hippocampus to refile fragmented memories, reducing their intrusive effects. EMDR has been shown to decrease PTSD symptoms, improve emotional regulation, and enhance cognitive functioning. It is particularly effective for individuals who struggle with flashbacks or nightmares, offering a pathway to long-term recovery and emotional resilience.
Cognitive-Behavioral Therapy (CBT) for Trauma
Cognitive-Behavioral Therapy (CBT) is a widely used, evidence-based approach for trauma recovery. It helps individuals identify and change negative thought patterns and behaviors linked to traumatic experiences. By focusing on the connection between thoughts, emotions, and actions, CBT empowers individuals to reframe unhelpful beliefs and develop coping strategies. This therapy is particularly effective in reducing symptoms of anxiety, depression, and PTSD. CBT also strengthens the prefrontal cortex, enhancing executive functioning and decision-making. Its structured, goal-oriented nature makes it adaptable to various types of trauma, providing a clear path toward healing and long-term emotional resilience.
Mindfulness and Trauma Recovery
Mindfulness practices offer a powerful tool for trauma recovery by fostering present-moment awareness and emotional regulation. Techniques such as meditation and deep breathing help calm the overactive amygdala, reducing stress and anxiety. Mindfulness strengthens the prefrontal cortex, enhancing self-regulation and resilience. It also promotes neuroplasticity, allowing the brain to rewire and heal. By encouraging non-judgmental acceptance of emotions and thoughts, mindfulness helps individuals process traumatic memories without becoming overwhelmed. This approach complements other therapies, providing a holistic path toward healing and emotional balance, and empowering individuals to reclaim control over their mental and emotional well-being in a gentle, sustainable way.
Neurofeedback and Brain Training
Neurofeedback, a form of biofeedback, helps individuals monitor and control their brain activity, promoting self-regulation and emotional stability. This non-invasive approach is particularly effective for trauma recovery, as it targets dysregulated brain regions. By training the brain to operate in healthier frequency ranges, neurofeedback reduces symptoms like anxiety and hyperarousal. It also enhances cognitive functioning and emotional resilience. Brain training exercises complement neurofeedback by strengthening neural pathways, improving focus, and boosting memory. Together, these techniques empower individuals to manage trauma-related challenges, fostering long-term recovery and mental well-being. Neurofeedback and brain training offer a powerful, non-pharmacological approach to healing the traumatized brain.

The Role of Neuroplasticity in Recovery
Neuroplasticity enables the brain to reorganize neural pathways, compensating for trauma-induced damage and facilitating recovery through improved cognitive and emotional functioning.
How the Brain Heals After Trauma
The brain’s healing after trauma involves neuroplasticity, where neural pathways reorganize to compensate for damaged areas. The hippocampus processes traumatic memories, reducing their distressing impact over time. The prefrontal cortex gradually regains its ability to regulate emotions and thoughts. Therapies like EMDR and mindfulness enhance this natural recovery process by promoting neural adaptation and emotional resilience. With time and support, the brain can rewire itself, leading to improved cognitive and emotional functioning. Understanding this healing process emphasizes the importance of patience and targeted interventions in trauma recovery.
Neuroplasticity and the Recovery Process
Neuroplasticity, the brain’s ability to reorganize itself, plays a crucial role in trauma recovery. Through this process, new neural pathways form, strengthening areas damaged by trauma. Therapies like EMDR and CBT guide the brain in rewiring, enhancing emotional regulation and cognitive functioning. Over time, the brain adapts, reducing the intensity of traumatic memories. Recovery is influenced by factors like trauma severity, individual resilience, and support systems. While progress varies, neuroplasticity offers hope for healing, demonstrating the brain’s remarkable capacity to adapt and recover from traumatic experiences with appropriate interventions and care.

The Impact of Trauma on Daily Life
Trauma disrupts emotional stability, relationships, and daily functioning, often causing heightened stress responses and difficulty managing routine tasks, significantly affecting overall quality of life and well-being.
Behavioral Changes and Trauma
Trauma often leads to significant behavioral changes, as the brain adapts to survive stressful events. Individuals may exhibit hypervigilance, avoidance of triggers, or heightened startle responses. Emotional regulation becomes challenging, with increased irritability or numbness. The prefrontal cortex, responsible for decision-making, may be underactivated, leading to impulsive behaviors. Conversely, the amygdala, the brain’s alarm system, becomes overactivated, intensifying fear responses. These changes can disrupt daily routines, relationships, and overall well-being. Understanding these behavioral shifts is crucial for providing support and facilitating recovery. Trauma’s impact on the brain highlights the need for compassionate approaches to address its long-lasting effects on behavior and emotional health.
Interpersonal Relationships and Trauma
Trauma significantly impacts interpersonal relationships, often leading to challenges in trust, intimacy, and communication. The brain’s altered emotional regulation and heightened stress responses can make it difficult to form and maintain healthy connections. Individuals may struggle with feelings of mistrust or emotional numbing, stemming from the overactivation of the amygdala and underactivation of the prefrontal cortex. These changes can result in withdrawal or lashing out, straining relationships. Understanding the neurological effects of trauma on social interactions is essential for fostering empathy and support. By addressing these challenges, individuals and their loved ones can work toward rebuilding and strengthening their relationships.
Societal Implications of Trauma
Trauma’s societal impact includes increased healthcare costs, reduced productivity, and higher rates of mental health disorders, placing a significant burden on communities and economic systems globally.
The Prevalence of Trauma in Society
Trauma is a widespread issue affecting individuals across all demographics. Its prevalence is linked to various factors, including adverse childhood experiences, violence, and natural disasters. Research indicates that trauma impacts brain development, leading to long-term mental and physical health challenges. Societal costs include increased healthcare expenses, lost productivity, and strained social services. Understanding trauma’s prevalence is crucial for developing effective prevention and intervention strategies. By addressing trauma at its root, societies can reduce its pervasive effects and foster resilience. This requires a collective effort to raise awareness and implement trauma-informed care practices.
The Economic and Social Costs of Trauma
Trauma imposes significant economic and social burdens on individuals and society. Healthcare costs rise due to mental health disorders, chronic illnesses, and substance abuse linked to trauma. Lost productivity and workplace absenteeism further strain the economy. Socially, trauma disrupts relationships, reduces academic performance, and increases crime rates. The emotional toll on families and communities exacerbates these challenges. Addressing trauma requires comprehensive interventions to mitigate its far-reaching consequences and promote societal well-being. Understanding these costs underscores the importance of early intervention and trauma-informed care to reduce long-term economic and social impacts.
Resources for Understanding and Addressing Trauma
Explore recommended readings, online courses, and workshops to deepen your understanding of trauma and recovery. Resources like EMDR therapy and neurofeedback offer practical tools for healing and education.
Recommended Reading on Trauma and the Brain
A comprehensive guide to understanding trauma’s impact on the brain, this resource explores neurobiological changes, recovery strategies, and therapeutic approaches. Discover how trauma affects brain regions like the amygdala, hippocampus, and prefrontal cortex. Learn about EMDR therapy, mindfulness, and neurofeedback as effective tools for healing. The guide also delves into the role of neuroplasticity in recovery, offering insights into how the brain can rewire and heal. Perfect for professionals and individuals seeking to understand trauma’s complexities, this reading provides evidence-based strategies for addressing trauma’s effects on mental and physical health. A must-read for anyone looking to deepen their knowledge of trauma and its brain-based implications.
Online Courses and Workshops on Trauma Recovery
Explore online courses and workshops designed to deepen understanding of trauma recovery. These resources offer insights into neurobiology, therapeutic techniques, and practical strategies for healing. Topics include EMDR therapy, mindfulness, and cognitive-behavioral approaches. Many courses are led by experts like Dr. Kerry Ressler, providing evidence-based methods for addressing trauma. Workshops often focus on skills for emotional regulation, memory processing, and rebuilding neural pathways. Whether for professionals or individuals, these programs provide accessible learning opportunities to understand and address trauma’s impact on the brain. They also include interactive elements like webinars and forums, fostering a supportive environment for growth and recovery.
